Hashimoto’s Thyroiditis – Understanding the Condition
Get expert insights about Hashimoto’s Thyroiditis, including its causes, symptoms, diagnosis, and treatment options. The information on this site is curated with the support of Team MACS Clinic and Dr. Sandeep Nayak, a globally acclaimed surgical oncologist in India specializing in head and neck surgery. He is recognized for pioneering the Advanced RABIT technique for Robotic Thyroidectomy, which has made significant strides in minimally invasive thyroid surgeries. Stay informed with our regularly updated information on this site to better understand and manage thyroid conditions effectively.
hypothyroidism. Globally, around 5% of the population is affected by this condition. It is increasingly prevalent in India, where approximately 11% of individuals, especially women, experience thyroid-related issues. If you’re suffering from this condition, there are solutions. Early diagnosis and personalized treatment for underactive thyroid can significantly improve the patient’s quality of life.
Have a Question?
Don’t let thyroid problems go unnoticed. Get expert advice and understand your treatment options. Book an appointment now!
What is Hashimoto’s Thyroiditis?
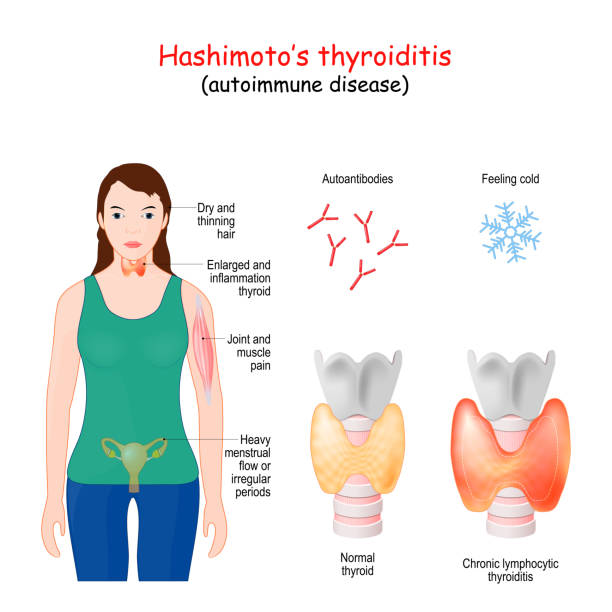
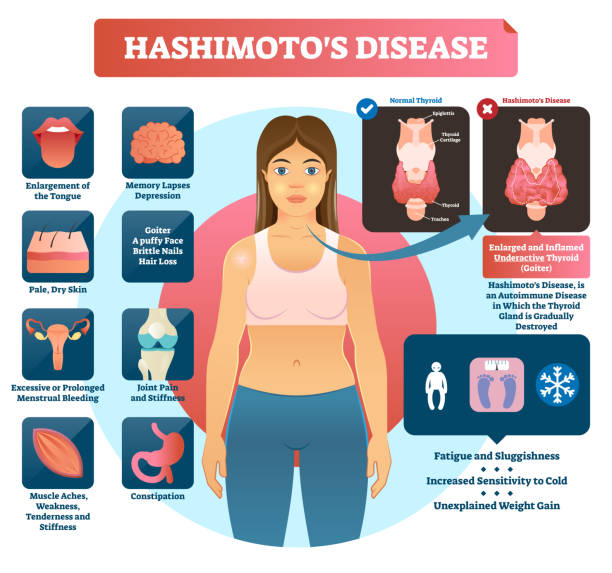
Hashimoto’s Thyroiditis, also referred to as chronic lymphocytic thyroiditis, is an autoimmune condition in which the immune system targets the thyroid gland. Over time, this leads to inflammation, disrupting the thyroid’s ability to produce hormones necessary for regulating metabolism. This condition is the leading cause of hypothyroidism. It primarily affects middle-aged women but can also occur in men and children.
The thyroid gland is crucial in regulating critical body functions like metabolism, heart rate, and temperature. Hence, untreated Hashimoto’s Thyroiditis can lead to more severe issues such as heart disease, mental health problems, and reproductive difficulties.
Curious about the reasons behind Hashimoto’s Thyroiditis? Let’s explore the factors that contribute to this condition.
Causes and Risk Factors
Hashimoto’s Thyroiditis occurs when the immune system mistakenly attacks the thyroid gland. The exact cause is unknown, but several factors increase the risk of developing this condition:
Genetics
A family history of thyroid or autoimmune diseases raises the likelihood of developing Hashimoto’s disease.
Hormonal changes
Women, especially during pregnancy or menopause, are more likely to develop Hashimoto’s Thyroiditis.
Radiation exposure
Previous exposure to radiation, especially in the head or neck area, can trigger thyroid problems.
Other autoimmune diseases
People with conditions like rheumatoid arthritis or type 1 diabetes are more prone to Hashimoto’s disease.
How does Hashimoto’s Thyroiditis present itself? Let’s dive into the signs you should watch for.
Symptoms of Hashimoto’s Thyroiditis
Hashimoto’s disease symptoms develop gradually, often going unnoticed until the condition worsens. Common signs include:

Fatigue
A persistent feeling of tiredness despite adequate rest.

Weight gain
Unexplained weight gain, even with no changes in diet or exercise.
Cold intolerance
Increased sensitivity to cold temperatures.

Hair loss
Thinning of hair or patchy hair loss.

Depression
Mood swings or feelings of sadness that seem unrelated to life events.

Memory issues
Difficulty concentrating or remembering things.
Have a Question?
Are you experiencing any of these symptoms? Consult a seasoned specialist for appropriate diagnosis and management.
Now, let’s explore the steps involved in diagnosing this thyroid condition.
Hashimoto’s Thyroiditis Diagnosis
Hashimoto’s disease symptoms develop gradually, often going unnoticed until the condition worsens. Common signs include:
Medical History Review

The doctor will review the patient’s medical history and ask about the symptoms of an underactive thyroid.
Physical Examination:

The specialist may check for an enlarged thyroid (goitre) and other physical signs of hypothyroidism, such as dry skin or facial puffiness.
Blood Tests

These tests measure hormone levels. Low thyroid hormone levels (T3 and T4) and high Thyroid-Stimulating Hormone (TSH) indicate hypothyroidism, a key sign of Hashimoto’s Thyroiditis.
Antibody Test

The presence of thyroid peroxidase (TPO) antibodies in the blood confirms an autoimmune response, which is typical for Hashimoto’s disease.
Imaging Tests

In some cases, an ultrasound may be recommended to check the size of the thyroid and detect any abnormalities.
Fine Needle Aspiration (FNA) Biopsy

If nodules or irregularities are detected, a biopsy may be conducted to rule out other conditions like cancer.
What is the treatment for underactive thyroid? Here’s what you should know.
Treatment Options
Hashimoto’s disease treatments focus on managing symptoms and restoring thyroid hormone levels. Standard treatment options include:
Thyroid Hormone Replacement Therapy
These tests measure hormone levels. Low thyroid hormone levels (T3 and T4) and high Thyroid-Stimulating Hormone (TSH) indicate hypothyroidism, a key sign of Hashimoto’s Thyroiditis.
Surgical Treatment
If the thyroid gland is severely damaged or if there’s a large goitre, experts may recommend surgery to remove part or all of the thyroid gland:
Partial Thyroidectomy
If the thyroid enlarges or forms nodules, the surgeon may perform a partial thyroidectomy. This involves removing a portion of the thyroid gland to alleviate pressure on nearby structures like the trachea or oesophagus.
Total Thyroidectomy
In cases where severe goitre, nodules, or cancer is present, a total thyroidectomy might be necessary. This procedure removes the entire thyroid gland. After this surgery, patients need lifelong hormone replacement therapy to compensate for the loss of thyroid function.
Robotic-Assisted Thyroidectomy
For eligible patients, Dr. Sandeep Nayak and team utilize minimally invasive surgical options, such as Robotic Assisted Breast-axillo Insufflated Thyroidectomy (RABIT). This less invasive approach provides a faster recovery with minimal scarring.
Only well-trained, experienced thyroid surgeons must perform this procedure. When executed by inexperienced or occasional thyroid surgeons, there is a risk of:
– Incomplete removal of the diseased thyroid gland
– Complications in preserving the vital structures of the thyroid gland
How can you effectively manage Hashimoto’s Thyroiditis? Let’s look at some practical strategies.
Managing Hashimoto’s Thyroiditis
Routine check-ups are essential for tracking thyroid hormone levels and adjusting medications.
Taking prescribed thyroid hormone replacement consistently helps maintain normal hormone levels and control symptoms.
A nutrient-rich diet, especially with selenium and iodine, supports thyroid health. Consulting a nutritionist can offer tailored advice.

Techniques like Yoga, mindfulness, or counselling help manage stress and improve overall well-being.
Regular physical activity boosts energy and aids weight management
Limit foods like soy and cruciferous vegetables that affect thyroid function
Stay vigilant for complications like heart disease or depression, seeking timely medical intervention.
Conclusion
Hashimoto’s Thyroiditis is a manageable condition with appropriate treatment and lifestyle adjustments. Regular monitoring and adherence to treatment plans are vital to managing this chronic condition and alleviating symptoms. For comprehensive care and support, seeking expertise from a seasoned professional can make a significant difference in your journey toward optimal health.
Have a Question?
Need help managing Hashimoto’s Thyroiditis? Reach out to an expert and take control of your health today. Schedule an appointment today!
Frequently Asked Questions
1. How does Hashimoto's Thyroiditis affect pregnancy?
Untreated Hashimoto’s Thyroiditis during pregnancy can lead to complications like preterm birth, miscarriage, and developmental issues in the baby.
2. Can Hashimoto Thyroiditis lead to cancer?
While rare, untreated or longstanding Hashimoto’s Thyroiditis may increase the risk of developing thyroid lymphoma.
3. What happens if Hashimoto Thyroiditis is left untreated?
If left untreated, this condition can lead to severe hypothyroidism, heart problems, mental health issues, and a condition called Myxedema.
4. How often should thyroid levels be checked if I have Hashimoto's Thyroiditis?
Once diagnosed, thyroid levels should be monitored every 6-12 months or as your doctor advises to ensure proper medication dosage.
5. How is Hashimoto's Thyroiditis different from Graves' disease?
Hashimoto’s Thyroiditis leads to hypothyroidism (underactive thyroid), while Graves’ disease causes hyperthyroidism (overactive thyroid).
Disclaimer: This page is for informational purposes and is not intended for promotional use.